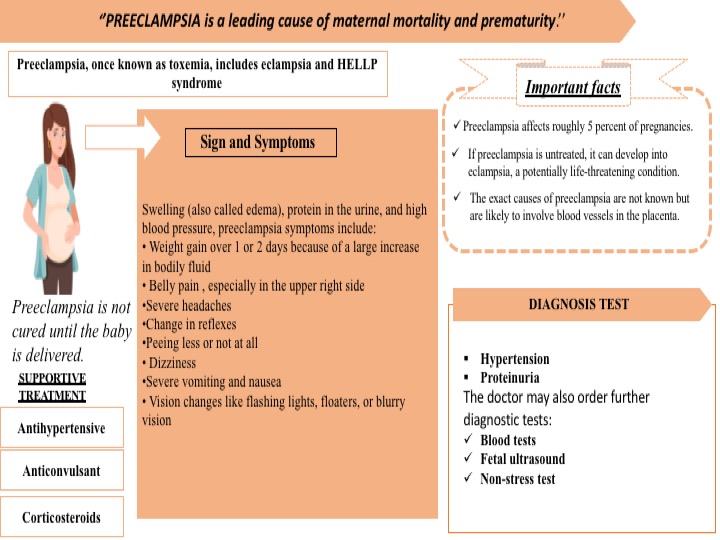
Pre-eclampsia is a leading cause of maternal mortality and prematurity. It is formerly called toxemia, which is when a pregnant woman has high blood pressure, protein in her urine, and swelling in her legs, feet, and hands. It can range from mild to severe. It usually happens late in the pregnancy after 20 weeks of pregnancy, though it can come earlier or just after delivery. In addition, there are several complications associated with preeclampsia such as HELLP syndrome, poor blood flow to the placenta & placental abruption, etc. Preeclampsia can lead to eclampsia, a serious condition that can have health risks for mom and baby and, in rare cases, cause death. Women with preeclampsia who have seizures have eclampsia. Approximately around 5% of all pregnant women get affected by preeclampsia.
The symptoms often begin after 34 weeks. Symptoms develop after birth, usually within 48 hours of delivery in few cases. They tend to go away on their own but can last up to 12 weeks after birth. In addition, the common symptoms develop such as edema, protein in the urine, and high blood pressure, preeclampsia symptoms include weight gain, belly pain, severe headaches, changes in reflexes, peeing less or not at all, dizziness, severe vomiting and nausea, vision changes like flashing lights, floaters, or blurry vision
Yet, the exact cause of preeclampsia is unidentified. But most of them say this problem happens with the development of the placenta because the blood vessels that supply it are narrower than normal and respond differently to hormonal signals. Because the blood vessels are narrower than normal, blood flow is limited. Several factors such as the history of preeclampsia, age, race, chronic hypertension, first pregnancy, obesity, and multiple pregnancies increase the chances of developing the preeclampsia
Preeclampsia is diagnosed through the following tests:
- Hypertension: The woman’s blood pressure is raised above 140/90 millimeters of mercury is abnormal in pregnancy.
- Proteinuria: Protein is detected in the urine is indicated for the severity of the condition.
The doctor may also recommend some further diagnostic tests:
- Blood tests – to assess the kidney and liver functions.
- Fetal ultrasound – to monitor the baby’s progress.
- Non-stress test – the doctor checks how the baby’s heartbeat reacts when they move. If the heartbeat increases 15 beats or more a minute for at least 15 seconds twice every 20 minutes, it is an indication that everything is normal
Recently, UniSA biomedical engineer Professor Benjamin Thierry developed a range of solid-state sensing and wearable technologies capable of diagnosing conditions including preeclampsia, epilepsy, fetal arrhythmias, and heart attacks. These wearables use a cutting-edge solid-state sensing technology called Field-Effect Transistors, which can measure bioelectric signals with extreme sensitivity when implemented at the nanoscale.”
However, Preeclampsia is not cured until the baby is delivered. Hence, the mother’s blood pressure comes down, she is at a greater risk of stroke, severe bleeding, separation of the placenta separates from the uterus and seizures. In some cases, especially if the preeclampsia started early, the delivery may not be the best option for the fetus.
Supportive therapy is recommended for the women Preeclampsia. Supportive therapy is as follows:
- Antihypertensives: These are used to lower blood pressure.
- Anticonvulsants: In severe cases, these drugs are used to prevent a first seizure. The doctor may prescribe magnesium sulfate.
- Corticosteroids: If the mother has preeclampsia or HELLP syndrome (see below) these drugs can improve platelet and liver functioning. This can prolong pregnancy.
While preeclampsia cannot be fully prevented, there are significant steps a woman can follow to avoid the moderate factors contribute to high blood pressure.
These may include:
- drinking between 6 and 8 glasses of water every day
- avoiding fried or processed food
- excluding added salt from the diet
- regular exercise
- avoiding alcohol and caffeine intake
- keeping the feet elevated a few times per day
- resting
- supplements and medications as prescribed by your doctor
